If you’re asking how to make PRF, you’re likely exploring regenerative medicine protocols or aesthetic treatments that rely on Platelet-Rich Fibrin (PRF). PRF is an autologous biological material derived from a patient’s own blood, widely used in dentistry, orthopedics, dermatology, and beauty clinics for tissue regeneration, wound healing, and skin rejuvenation. Unlike liquid concentrates, Platelet-rich plasma forms a fibrin matrix rich in platelets, white blood cells, and growth factors that support natural healing processes.
Preparing PRF consistently and effectively requires not only a solid understanding of the biological principles, but also the right tools — including high-quality PRF tubes and consumables. Because many products on the market vary in their additive composition, tube material, and manufacturing quality, clinics and laboratories often face uncertainty when selecting the best option to use.
What is PRF and why does it matter?
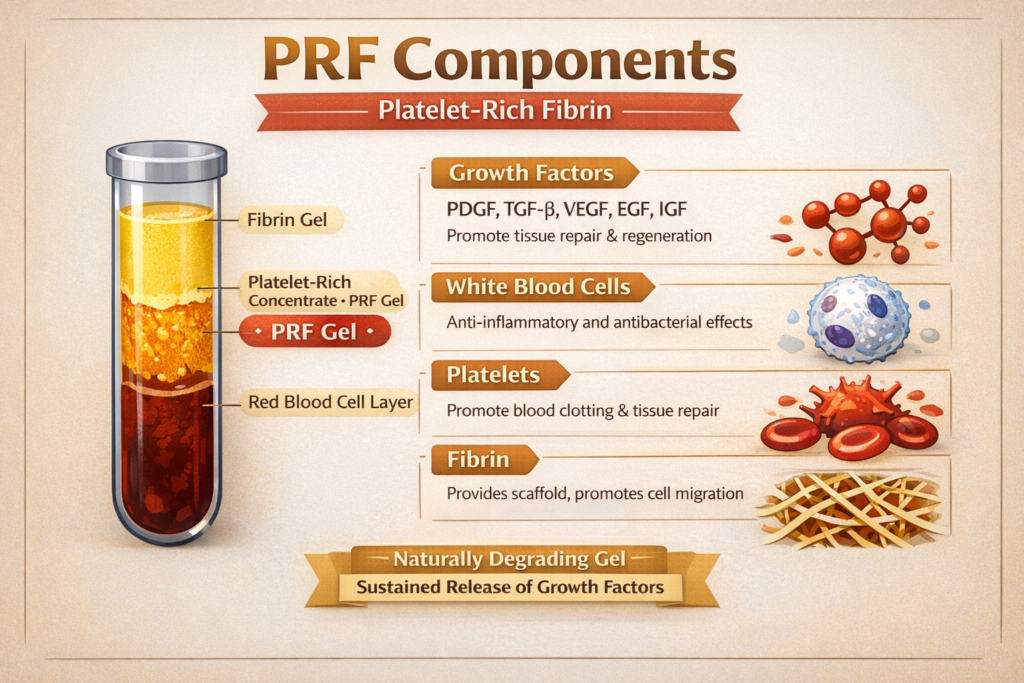
Before discussing how to make PRF, it helps to understand what PRF actually is and why it’s valuable. Platelet-rich plasma stands for Platelet-Rich Fibrin, a second-generation platelet concentrate that differs from earlier derivatives like PRP (Platelet-Rich Plasma) in key ways:
- PRF is produced without anticoagulants, allowing a natural fibrin clot to form.
- The fibrin matrix captures platelets, leukocytes, and stem cell precursors in a three-dimensional scaffold.
- This structure enables a sustained release of growth factors, such as PDGF, TGF-β, and VEGF, which support tissue repair, angiogenesis, and immune modulation.
This slow release makes Platelet-rich plasma particularly useful in procedures where a longer biological effect is desired, such as facial rejuvenation, hair restoration, dental implant integration, and wound healing. PRF uses the patient’s own blood and avoids bovine additives or anticoagulants. It is considered a safe and biocompatible option for regenerative treatments.
How to Make PRF?
Learning how to make PRF begins with understanding the correct preparation workflow. While specific protocols may vary slightly depending on clinic preferences, centrifuge equipment, and clinical goals, the following steps outline a standard procedure:
Step 1 — Blood Collection
Draw a defined volume of the patient’s blood into PRF tubes. These tubes should be specifically designed for Platelet-rich plasma preparation, often containing no anticoagulant or a minimal clotting modifier that allows natural fibrin formation. Choosing the right tube is a key part of consistent preparation and impacts yield and clot quality. If you are evaluating PRF consumables, you can explore product specifications and procurement support at Siny PRP.
Step 2 — Immediate Mixing
Unlike PRP preparation, PRF protocols usually avoid anticoagulants, so prompt processing is essential. Gently invert the tube if needed to ensure initial blood additive interaction, but avoid vigorous shaking that might disrupt cellular components.
Step 3 — Centrifugation
Place the tubes in a clinical centrifuge and run a pre-defined program. A typical Platelet-rich plasma protocol uses lower speeds (relative centrifugal force, or RCF) and shorter durations than standard blood fractionation:
- Lower speed helps maintain more platelets and leukocytes in the fibrin layer.
- Shorter spin times reduce premature clot compaction, yielding a more pliable fibrin matrix.
After centrifugation, the blood separates into layers: red blood cells at the bottom, a fibrin clot enriched with platelets in the middle, and platelet-poor plasma on top.
Step 4 — Clot Collection
Extract the PRF clot from the tube using sterile instruments. Depending on clinical intention, the clot can be used as:
- A plug or membrane for surgical or dental applications
- A topical application after microneedling or soft tissue procedures
- A fibrin-rich injection matrix, when combined with appropriate carrier techniques
Each form takes advantage of the fibrin matrix’s sustained release of growth factors and structural support.
PRF Applications
Once you understand how to make PRF, it’s helpful to know the applications that benefit most from its regenerative properties. PRF’s versatility stems from its ability to act as both a biological scaffold and a reservoir of growth factors:
Aesthetic and Dermatologic Use
In beauty clinics, Platelet-rich plasma is often used for facial rejuvenation, improving skin tone and texture, and reducing fine lines when applied after microneedling or injected into facial tissues. Its gradual release of growth factors supports gradual, natural tissue improvement.
Hair Restoration
PRF injections into the scalp aim to stimulate dormant hair follicles and promote hair thickness and density. As a biologically active product derived from the patient’s own blood, it is widely adopted in hair loss clinics seeking regenerative outcomes.
Dental and Oral Surgery
Dentists and oral surgeons may use Platelet-rich plasma as a membrane or graft adjunct to enhance bone and soft tissue healing around implant sites, extraction sockets, or periodontal defects.
Orthopedics and Wound Care
PRF is also applicable in musculoskeletal medicine, where it may support tendon, ligament, or chronic wound healing by delivering sustained growth factor signaling at the site of injury.
Each application benefits from the slow release of regenerative signals inherent to the fibrin matrix, a bioactive feature distinct from simpler liquid blood fractions.
Challenges and Best Practices in PRF Preparation
Understanding how to make PRF also involves acknowledging common challenges and ensuring best practices are followed:
- Timing Is Critical: PRF protocols often require immediate processing of collected blood to avoid premature clotting. Delays can reduce yield or affect clot quality.
- Standardization Matters: Variations in centrifuge calibration, tube quality, and handling technique can lead to inconsistent PRF preparations.
- Training and Technique: Proper training ensures that staff can consistently execute the workflow, from collection to application.
A frequent source of inconsistency is variation in consumables — particularly PRF tubes. Tubes with unstable vacuum force, inconsistent additives, or substandard materials may lead to unpredictable separation and reduced platelet yield. Partnering with a reliable supplier that provides consistent, validated Platelet-rich plasma tube products enhances procedure reproducibility and clinical confidence. For quality consumable options, specifications, and support. You are invited to explore Siny PRP or contact our team for personalized assistance.
Key Benefits of PRF Treatment
PRF treatment is widely adopted in aesthetic medicine, dentistry, and regenerative therapy because it offers several clear advantages over traditional platelet-based approaches. These benefits are closely linked to PRF’s biological properties and its natural preparation process.
1. 100% Autologous and Additive-Free
One of the most important features of Platelet-rich plasma is that it is completely autologous. It is prepared solely from the patient’s own blood and does not contain anticoagulants, preservatives, or synthetic additives. This significantly reduces the risk of allergic reactions or immune responses and makes PRF suitable for repeated clinical use.
2. Sustained Release of Growth Factors
Unlike liquid platelet concentrates, PRF forms a dense fibrin network that traps platelets and leukocytes within its structure. This allows growth factors to be released gradually over an extended period, supporting continuous tissue repair rather than a short-term biological stimulus. This sustained effect is especially beneficial for skin rejuvenation, wound healing, and bone regeneration.
3. Natural Fibrin Scaffold for Tissue Regeneration
The fibrin matrix in Platelet-rich plasma acts as a three-dimensional scaffold that supports cell migration, angiogenesis, and collagen formation. This structure helps stabilize the treatment area and creates an environment conducive to natural healing. Which is one reason Platelet-rich plasma is commonly used in surgical and post-procedural applications.
4. Versatility Across Multiple Clinical Applications
PRF treatment can be applied in a wide range of procedures, including facial aesthetics, hair restoration, dental implants, periodontal therapy, and orthopedic support. It can be used alone or combined with other treatments such as microneedling or grafting techniques, allowing clinicians to tailor protocols based on individual patient needs.
5. Simple Preparation and Cost Efficiency
Once standardized, PRF preparation is relatively straightforward and does not require complex chemical formulations. This simplicity helps clinics improve workflow efficiency while maintaining high treatment quality. With proper training and consistent preparation methods, PRF can be integrated into daily practice without a significant operational burden.
When these features are fully understood and applied correctly, Platelet-rich plasma treatment delivers reliable and repeatable clinical outcomes. This is why many practitioners focus on optimizing both technique and preparation conditions to fully realize the benefits of PRF therapy.
FAQs
Q: What is the difference between PRF and PRP?
PRF forms a fibrin matrix that releases growth factors over time, while PRP remains a liquid concentrate with a more immediate but shorter release of factors.
Q: How long does it take to make PRF?
The preparation process, from blood draw to PRF extraction, typically takes around 10–15 minutes, depending on centrifugation parameters.
Q: Do I need a special tube to make PRF?
Yes, tubes designed for PRF preparation help ensure proper clot formation and platelet preservation. Consistent tube quality supports repeatable Platelet-rich plasma results.
Q: Can PRF be used immediately after preparation?
Yes. PRF is generally used immediately after centrifugation for clinical applications.
Q: Why should I care about supplier quality when learning how to make PRF?
Supplier quality affects tube material, additive consistency, and performance, all of which influence Platelet-rich plasma yield and clinical effectiveness. Clinics should evaluate product specifications carefully, and you can contact Siny PRP for detailed support and recommendations.
Summary
Understanding how to make PRF is not just about following a centrifugation protocol—it’s about mastering the full process, from blood collection and handling to choosing the right consumables and applying PRF correctly in clinical practice. Platelet-rich plasma stands out as a powerful regenerative material due to its natural fibrin matrix, sustained growth factor release, and excellent biocompatibility across aesthetic, dental, and medical applications.
Consistent PRF results depend heavily on standardization, staff training, and especially the quality of Platelet-rich plasma tubes used during preparation. Variations in tube materials, additives, or vacuum stability can directly impact clot structure, platelet retention, and overall treatment outcomes. For clinics and distributors aiming to scale PRF treatments reliably, working with an experienced and quality-focused supplier is a strategic decision rather than a simple purchasing choice.
By combining sound clinical knowledge with dependable Platelet-rich plasma consumables, practitioners can achieve predictable regenerative results while improving workflow efficiency and patient satisfaction. For those evaluating PRF tube solutions or seeking technical guidance, exploring professional options and support through Siny PRP can be a practical next step.