What is PRF in Orthopaedics?
What is PRF in Orthopaedics?Platelet-Rich Fibrin (PRF) is an autologous blood product that separates blood drawn from the patient’s veins. PRF is a second-generation platelet concentrate that contains a high concentration of platelets and a significant amount of fibrin, leukocytes, and various growth factors. These components work together to accelerate tissue repair and regeneration, making PRF an important biomaterial.
Preparation Method of PRF
The preparation of PRF is relatively simple and involves the following steps:
- Blood Drawing: A specific amount of blood, typically 10-20 milliliters, is drawn from the patient’s vein.
- Centrifugation: The drawn blood is placed in a tube without anticoagulants and centrifuged at a low speed (usually 2700 RPM) for about 12 minutes. During this process, the platelets and fibrin in the blood gradually aggregate to form a gel-like substance.
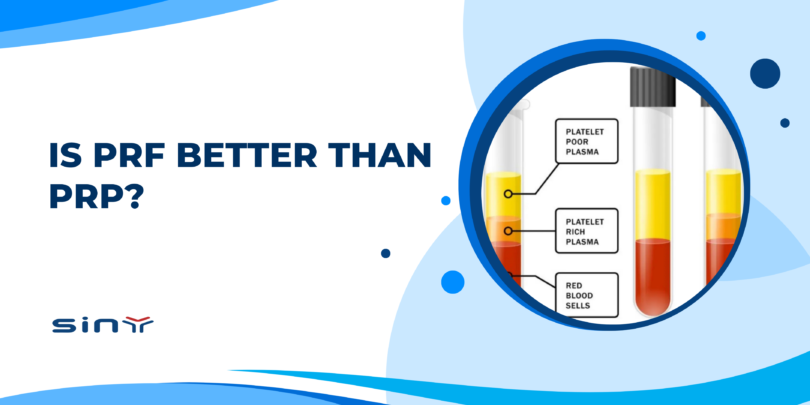
- Collection of PRF: After centrifugation, the blood in the tube separates into three layers: the top layer is serum, the middle layer is platelet-rich fibrin gel (PRF), and the bottom layer is red blood cells. The middle PRF layer is carefully extracted using sterile tools for clinical use.
Since no anticoagulants are used during the preparation of PRF, the blood naturally coagulates during centrifugation, forming a three-dimensional fibrin network. This structure helps slow down the release of growth factors, extending their action duration.

Pre-treatment Preparation
Before undergoing PRF treatment, patients need to go through several preparatory steps:
- Comprehensive Examination: Physicians perform a thorough physical examination and medical history analysis to determine if the patient is suitable for PRF treatment.
- Blood Drawing Preparation: Patients should avoid medications that affect blood coagulation, such as aspirin, before blood drawing. Additionally, maintaining good nutrition and rest is essential to ensure high-quality blood.
- Sterile Procedure: All procedures involving blood drawing and PRF preparation must be conducted in a sterile environment to prevent infection.
- Informed Consent: Before treatment, the physician should explain the procedure, expected outcomes, and potential risks to the patient and obtain informed consent.
Treatment Cycle
The PRF treatment cycle varies based on the patient’s condition and treatment goals. Generally, PRF treatment involves several stages:
- Initial Treatment: During the initial treatment, the prepared PRF is applied to the affected area, such as joints, bone defects, or soft tissue injuries. This process typically takes 30-60 minutes.
- Follow-up Treatments: After the initial treatment, patients need regular follow-ups to assess the treatment’s effectiveness and recovery progress. Depending on the situation, the physician may recommend multiple PRF treatments, usually spaced 4-6 weeks apart.
- Long-term Monitoring: Post-treatment, patients should undergo regular check-ups to ensure the treatment’s lasting effects and prevent recurrence.
Application of PRF in Orthopedics
PRF’s application in orthopedics mainly focuses on joint repair, bone defect filling, and soft tissue repair. Specific applications include:
- Joint Repair: PRF can be used to treat joint cartilage injuries. The abundant growth factors in PRF stimulate the proliferation and differentiation of cartilage cells, promoting cartilage tissue repair and regeneration.
- Bone Defect Filling: In fracture repair and bone defect filling, PRF serves as a bioactive scaffold. It fills bone defect areas and promotes new bone tissue growth and healing by releasing growth factors.
- Soft Tissue Repair: PRF is also widely used in soft tissue repair, such as ligaments and tendons. Its application can reduce postoperative complications and accelerate recovery.
Advantages of PRF in Orthopedics
- Promotes Tissue Regeneration: PRF is rich in growth factors such as Transforming Growth Factor-β (TGF-β), Platelet-Derived Growth Factor (PDGF), and Insulin-like Growth Factor (IGF), significantly promoting tissue regeneration and repair.
- Reduces Inflammatory Response: The leukocytes and anti-inflammatory factors in PRF help reduce inflammation, which is crucial for postoperative recovery.
- No Immune Rejection: As an autologous blood product, PRF does not cause immune rejection, significantly enhancing safety.
- Simple and Convenient: The preparation process of PRF is simple, requiring only centrifugation. It is easy to use and widely applicable.
Comparison of PRF and PRP
Platelet-Rich Plasma (PRP) is a first-generation platelet concentrate. While it also contains a high concentration of growth factors, PRP and PRF differ in several ways. PRP preparation requires anticoagulants, whereas PRF does not, making PRF preparation simpler. Secondly, in terms of composition, PRF contains a high concentration of platelets and a significant amount of fibrin and leukocytes, which are relatively scarce in PRP. The presence of fibrin in PRF provides a better scaffold for cell attachment and proliferation. Additionally, the growth factors in PRP are released quickly, whereas PRF, with its fibrin network, allows for a slow release, extending the duration of action and benefiting long-term tissue repair and regeneration. Finally, due to its more diverse cell and growth factor composition, PRF generally shows superior effects in promoting tissue regeneration and repair compared to PRP. Therefore, PRF demonstrates more significant advantages in clinical applications, especially in orthopedics.
Conclusion
As an emerging biomaterial, PRF has broad application prospects in orthopedic joints. It effectively promotes tissue regeneration and repair, reduces inflammatory responses, avoids immune rejection, and is simple to prepare. Compared to traditional PRP, PRF shows significant advantages in composition, duration of action, and clinical effectiveness. Consequently, the application of PRF in orthopedic joints is expected to become increasingly widespread, offering patients more treatment options and better recovery outcomes.