How Do PRP Injections Work? In the rapidly advancing field of regenerative medicine, Platelet-Rich Plasma (PRP) therapy has established itself as a cornerstone treatment for a variety of clinical applications, from orthopedics to aesthetic medicine. For private clinics, healthcare professionals, and medical supply distributors, a fundamental understanding of the science behind this autologous treatment is paramount. The question, How do PRP injections work?, goes beyond a simple explanation; it delves into a complex biological process that, when properly harnessed, can significantly enhance patient outcomes.
What is the mechanism of PRP therapy?
To comprehend how PRP injections function, one must first appreciate the intricate role of platelets in the body’s natural healing cascade. Platelets, or thrombocytes, are small, anucleated cell fragments in the blood, primarily known for their role in hemostasis. However, their contribution to tissue repair is far more profound. Platelets contain numerous intracellular granules, which are reservoirs for a multitude of growth factors and cytokines. When an injury occurs, platelets are among the first responders, becoming activated and releasing these potent signaling molecules at the site of damage.
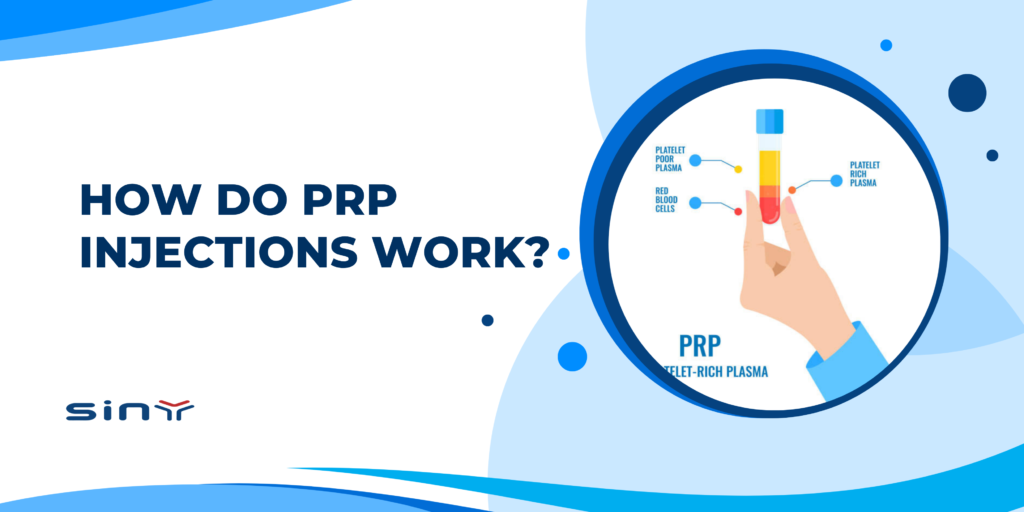
PRP therapy leverages this natural process by creating a supra-physiological concentration of platelets. The procedure involves drawing a patient’s own blood, which is then processed to separate the platelets and plasma from red and white blood cells. The resulting Platelet-Rich Plasma is a concentrate of platelets, often five to ten times greater than that of normal blood. When this concentrate is injected into injured or degenerated tissue, the activated platelets release a powerful cocktail of growth factors, including:
- Platelet-Derived Growth Factor (PDGF): Promotes cell replication, angiogenesis (the formation of new blood vessels), and tissue remodeling.
- Transforming Growth Factor-beta (TGF-β): Stimulates the synthesis of collagen and other extracellular matrix proteins, crucial for tissue structure.
- Vascular Endothelial Growth Factor (VEGF): A key mediator of angiogenesis, improving blood supply to the injured area.
- Epidermal Growth Factor (EGF): Encourages cell growth, proliferation, and differentiation.
- Fibroblast Growth Factor (FGF): Contributes to tissue repair and cell proliferation.
The collective action of these growth factors orchestrates a multi-phase healing response. They attract stem cells and other reparative cells to the site of injection, reduce harmful inflammation, and stimulate the proliferation and differentiation of local cells to regenerate and repair damaged tissues like tendons, ligaments, cartilage, and skin.

The Critical Role of the PRP Preparation Process
The therapeutic potential of PRP is only realized if the preparation process is precise and optimized. The journey from whole blood to a potent autologous biologic is a multi-step procedure that demands meticulous attention to detail and high-quality equipment. The standard process involves three key stages: blood collection, centrifugation, and extraction of the PRP. Each stage is a critical control point that influences the final product’s platelet concentration, purity, and ultimately, its clinical efficacy.
The centerpiece of this process is centrifugation. After the initial blood draw into specialized tubes containing an anticoagulant, the sample is placed in a centrifuge. This machine spins at high speeds, creating forces that separate the blood components based on their density. Red blood cells, being the densest, form a layer at the bottom. The least dense component, the plasma, forms the top layer. In between is the “buffy coat,” a thin layer rich in platelets and white blood cells. The specific protocol—including the speed, time, and temperature of the centrifugation cycle—is a determining factor in the quality of the resulting PRP. Different protocols can yield PRP with varying concentrations of platelets and leukocytes, which may be desirable for different clinical applications.
Why High-Quality PRP Tubes Are Non-Negotiable for Efficacy
While the centrifuge provides the force for separation, the PRP tube is the vessel where the critical separation occurs. The quality and design of this single-use medical device are profoundly important and can significantly impact the final PRP concentrate. A substandard tube can compromise the entire procedure, leading to a suboptimal therapeutic product and diminished patient results. Key features to consider in a PRP tube include the type of anticoagulant used, the presence and quality of a separating gel, and the biocompatibility of the material.
The anticoagulant, for example, must effectively prevent clotting without altering platelet function. The separating gel, if present, must form a stable barrier between the red blood cells and the plasma during centrifugation, allowing for easy and precise extraction of the platelet-rich layer while minimizing contamination. Red blood cell contamination can lead to increased post-injection inflammation and pain. Therefore, the efficacy of the entire procedure, which hinges on how PRP injections work, is fundamentally dependent on the quality and reliability of the prepared plasma. Investing in superior PRP tubes is an investment in consistency, safety, and clinical excellence. To ensure your practice is delivering the highest standard of care, it is crucial to partner with a supplier that prioritizes quality and consistency. Explore the advanced features of our PRP tubes on the Siny PRP product page.
Clinical Applications and Maximizing Patient Outcomes
The well-documented mechanism of PRP has led to its successful application across a wide spectrum of medical disciplines. In orthopedics and sports medicine, clinicians use PRP injections to treat chronic tendon injuries, ligament sprains, and osteoarthritis, helping patients reduce pain and improve function. In dermatology and aesthetics, practitioners apply PRP for its regenerative properties in hair restoration and skin rejuvenation, stimulating hair follicles and promoting collagen production. The success in these varied applications all traces back to the fundamental way PRP stimulates the body’s cellular repair mechanisms.
For clinics and distributors, this versatility represents a significant opportunity. However, to build a reputable and successful regenerative medicine service, achieving consistent and positive patient outcomes is essential. This consistency is born from a combination of proper patient selection, skilled injection technique, and an unwavering commitment to using high-quality medical consumables. The choice of a PRP system, particularly the PRP tubes, is a critical decision that influences the viability and concentration of platelets in the final injectate. A reliable supplier provides more than just a product; they provide a guarantee of quality that translates into more predictable and effective treatments for patients. Partnering with a trusted supplier is key to building a successful regenerative medicine practice. Contact Siny PRP today to learn how our products can enhance your clinical offerings.
FAQs
1. What is the optimal platelet concentration for effective PRP therapy?
While there is no single universally agreed-upon standard, most research suggests that a platelet concentration of 3 to 5 times the baseline level in whole blood is effective for stimulating tissue repair. The ideal concentration can also vary depending on the specific condition being treated.
2. What are the key features to look for in a high-quality PRP tube?
Look for tubes made from high-grade, biocompatible materials that are sterile and non-pyrogenic. Key features include an effective anticoagulant that preserves platelet integrity and a high-quality, thixotropic separation gel that provides a clean separation of red blood cells from the plasma, ensuring a high platelet yield and purity.
3. How does the choice of anticoagulant in the PRP tube impact the final product?
The anticoagulant (e.g., Sodium Citrate or ACD-A) is crucial for preventing the blood from clotting after it’s drawn. A proper anticoagulant should be effective in its primary role without damaging the platelets or interfering with their ability to become activated and release growth factors upon injection into the target tissue.
4. Why is a consistent centrifugation protocol so important for PRP preparation?
A consistent and validated centrifugation protocol (both speed and time) is essential for producing a consistent end product. Variations in the protocol can lead to significant differences in platelet concentration and the level of red and white blood cell contamination, which in turn affects the therapeutic quality and predictability of the treatment.
5. How can a reliable supplier impact the success of my clinic’s PRP services?
A reliable supplier like Siny PRP provides consistently high-quality, sterile, and effective PRP tubes, which are fundamental to preparing a potent PRP product. This consistency translates to more predictable and reliable clinical outcomes, enhancing patient satisfaction and the reputation of your practice. A good supplier also ensures a stable supply chain and provides excellent customer support.