Why Can PRP Be Used for Wound Dressing? Chronic, non-healing wounds remain a common and challenging problem in clinical practice, such as diabetic foot ulcers, venous leg ulcers, pressure injuries, burns, and radiation-induced skin damage. These wounds often heal slowly due to poor blood supply, infection, or impaired tissue repair mechanisms, and can significantly affect patients’ quality of life.
Traditional wound care mainly focuses on protecting the wound surface, maintaining a moist environment, and preventing infection. While these measures provide basic support, they do not strongly activate the body’s repair processes.
Platelet-Rich Plasma (PRP), with its high platelet concentration and abundant growth factors, has shown unique advantages in promoting tissue regeneration. In recent years, researchers have developed PRP into gels, membranes, and combinations with other materials for use as wound dressings, making it a promising tool in regenerative medicine.
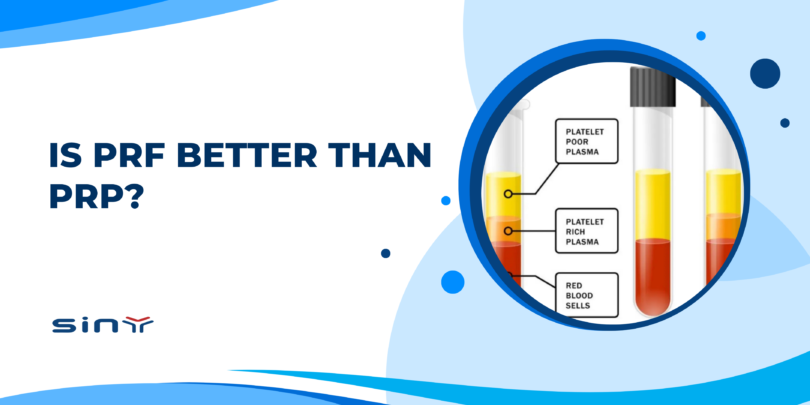
What Is PRP?
Technicians prepare PRP from a patient’s venous blood through centrifugation, producing plasma with a platelet concentration typically 3–5 times higher than normal levels, and in some techniques up to 7–10 times higher. Platelets contain α-granules that store multiple growth factors and cytokines, including:
- PDGF (Platelet-Derived Growth Factor) stimulates fibroblast and smooth muscle cell proliferation.
- VEGF (Vascular Endothelial Growth Factor) – promotes angiogenesis and improves local blood supply.
- EGF (Epidermal Growth Factor) – accelerates keratinocyte migration and epithelial coverage.
- TGF-β (Transforming Growth Factor-β) regulates cell differentiation and promotes collagen synthesis.
- IGF (Insulin-Like Growth Factor) – supports cell repair and metabolism.
Because PRP is autologous, it carries minimal risk of immune rejection and offers excellent biocompatibility, making it suitable for various wound care applications.

How PRP Works in Wound Dressings
- Stimulating Cell Proliferation and Migration: PDGF, EGF, and other factors in PRP activate fibroblasts and keratinocytes, accelerating epithelialization.
- Promoting Angiogenesis: VEGF and similar growth factors induce new capillary formation, improving oxygen and nutrient delivery to the wound bed.
- Regulating Inflammation: PRP contains anti-inflammatory cytokines that help control excessive inflammation, reduce swelling and exudation, and shorten the inflammatory phase.
- Enhancing Collagen Production and Tissue Remodeling: TGF-β promotes collagen deposition and alignment, strengthening newly formed tissue and reducing the risk of wound reopening.
- Providing a Moist, Bioactive Healing Environment: PRP dressings maintain a moist surface while continuously releasing bioactive molecules that act directly on the wound bed.
Clinical Evidence and Research Findings
- Diabetic Foot Ulcers – Multiple studies have shown that PRP significantly improves complete healing rates and shortens healing time. A Mayo Clinic review reported that patients treated with PRP had better outcomes within 8 weeks compared to standard care.
- Venous Leg Ulcers – PRP dressings have been shown to reduce wound size, promote granulation tissue growth, and relieve pain.
- Surgical Incisions and Skin Grafts – In plastic and burn surgery, PRP accelerates both donor and recipient site healing, while reducing postoperative swelling and infection risk.
- Radiation Injuries and Burns – PRP supports microvascular repair, improving recovery in radiation-damaged skin and deep burn injuries.
Advantages and Limitations
Advantages
- High safety – Autologous origin minimizes the risk of immune rejection.
- Faster healing – Rich in multiple growth factors that promote tissue repair at multiple stages.
- Versatile application forms – Can be used as gels, membranes, sponges, or combined with other dressing materials.
- Reduced scarring – Encourages organized collagen deposition for better-quality healing.
Limitations
- Lack of standardization – Different centrifugation protocols and devices produce variable platelet concentrations.
- Technical requirements – Preparation must be done under sterile conditions by trained personnel.
- Cost – Higher preparation and application costs compared to conventional dressings.
Applications
PRP dressings are commonly used for:
- Chronic ulcers (diabetic foot, venous leg ulcers, pressure injuries)
- Post-surgical incision care
- Burn and skin graft donor/recipient sites
- Radiation-induced skin damage
- Traumatic wounds (including skin tears from sports injuries)
FAQs
1. Is PRP wound dressing safe?
Yes. Since the patient’s blood provides the PRP, it poses minimal risk of immune rejection or allergic reactions.
2. What types of wounds are suitable for PRP dressings?
They are especially suitable for slow-healing wounds, wounds with poor blood supply, or those needing faster recovery, such as diabetic foot ulcers, burns, and surgical incisions.
3. How long does it take to see results with PRP dressings?
Most patients observe faster granulation tissue growth and noticeable wound size reduction within 2–4 weeks.
4. Is PRP preparation painful?
Preparation involves drawing a small amount of venous blood. Discomfort is minimal, and most patients tolerate it well.
Summary
PRP dressings deliver a high concentration of platelets that release multiple growth factors, stimulating cell proliferation, promoting angiogenesis, regulating inflammation, and maintaining a moist, bioactive environment for healing. While standardization and cost remain challenges, PRP has demonstrated proven benefits in chronic wound care, surgical recovery, and trauma management. With continued advances in preparation techniques and clinical evidence, PRP is likely to become a core component of future wound care strategies.