PRP, which stands for Platelet-Rich Plasma, has gained attention as a promising treatment for arthritis. Arthritis significantly affects the quality of life, and traditional treatments like medication, physical therapy, and surgery often fall short of repairing joint damage. Advances in regenerative medicine have led many professionals to explore PRP as a way to activate the body’s natural repair processes. This article explains the basics of PRP, its preparation, how arthritis develops, the treatment’s working mechanism, clinical outcomes, and future research directions. Our goal is to provide a clear and professional resource for medical staff, patients, and industry peers.
2. Basic Concepts of PRP
2.1 Definition and Types
PRP is a plasma sample enriched with platelets, obtained by drawing the patient’s blood and processing it with a centrifuge. Platelets contain several growth factors such as TGF-β, PDGF, and IGF. These factors play an important role in tissue repair and inflammation control.
PRP generally comes in two forms:
- Leukocyte-rich PRP: This type contains more white blood cells and may help regulate local immune responses.
- Leukocyte-poor PRP: This form focuses on promoting cartilage repair while reducing local inflammation.
2.2 Preparation Process
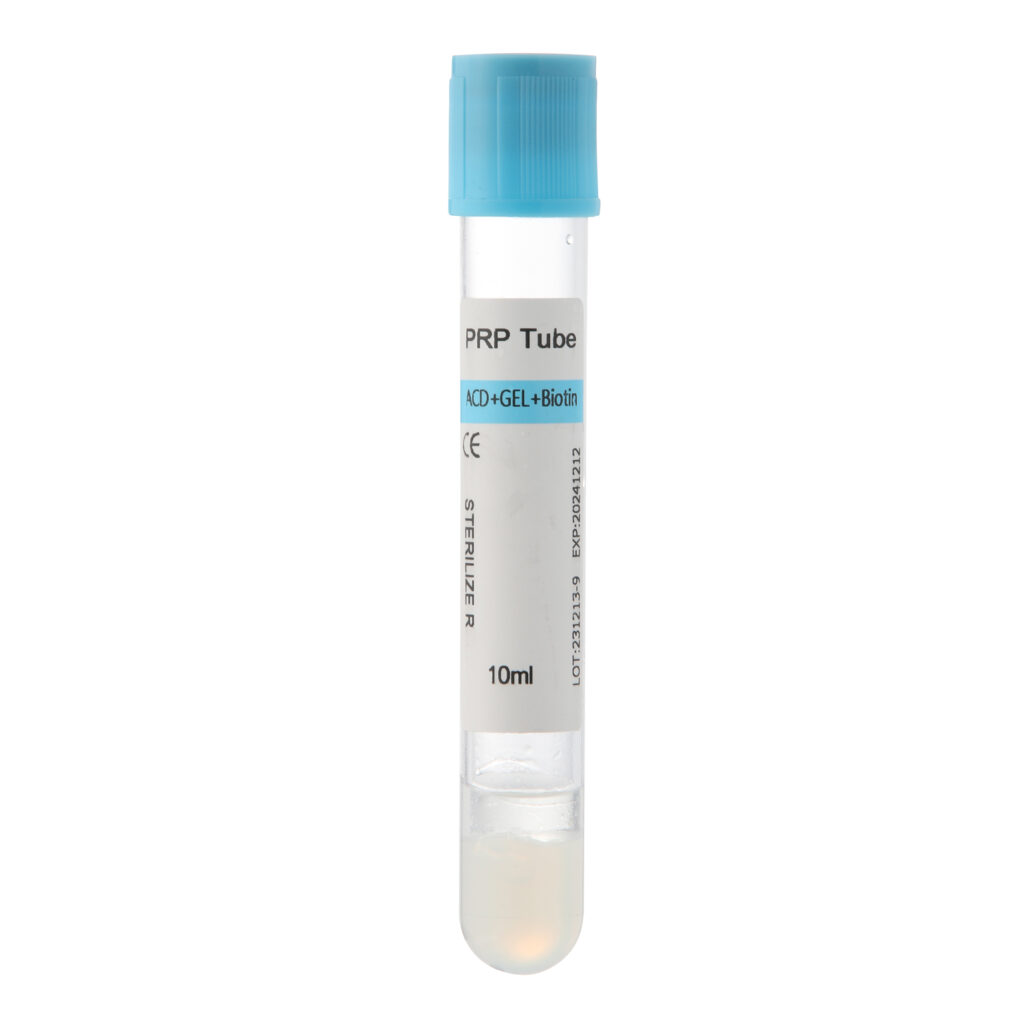
The preparation of PRP involves these key steps:
- Blood Collection: Draw blood from the patient under sterile conditions.
- Centrifugation: Use a centrifuge to separate the blood into layers, isolating the platelet-rich plasma.
- Concentration: Further process the plasma to achieve the desired concentration of platelets and growth factors.
Different preparation methods can affect the final composition and activity of PRP, so choosing the right technique is crucial for effective treatment.
3. Arthritis: Pathology and Clinical Features
3.1 Types of Arthritis
Arthritis refers to joint and surrounding tissue inflammation. The main types include:
- Osteoarthritis: Common in older adults, it features the breakdown of joint cartilage, formation of bone spurs, and narrowing of the joint space.
- Rheumatoid Arthritis: This autoimmune condition causes inflammation in the joints and can affect other body systems.
3.2 Pathological Changes and Mechanisms
Arthritis involves several changes at the cellular and molecular levels:
- Cartilage Degradation: Continuous mechanical stress and inflammation reduce cartilage cell activity and accelerate the breakdown of the cartilage matrix.
- Synovial Inflammation: Synovial cells release inflammatory molecules like IL-1 and TNF-α, which sustain and worsen inflammation.
- Bone Alterations: The formation of bone spurs, hardening, and localized bone loss further restrict joint movement.
These processes lead to pain, stiffness, and limited mobility in affected individuals.
4. How PRP Works in Arthritis Treatment
4.1 Promoting Tissue Repair
PRP releases growth factors that support joint repair:
- TGF-β: Regulates cell differentiation and encourages the production of cartilage matrix proteins.
- PDGF: Enhances cell migration and proliferation, improving the condition of the damaged area.
- IGF: Supports cell growth and maintains metabolic balance, protecting cartilage cells.
4.2 Regulating Inflammation
PRP also helps reduce inflammation:
- Lowering Inflammatory Mediators: They decrease IL-1, TNF-α, and other pro-inflammatory substances, reducing inflammation in the synovial membrane.
- Enhancing Blood Flow: PRP promotes the formation of new blood vessels, increasing nutrient and oxygen delivery to the affected tissues.
4.3 Modulating Immune Response
PRP can adjust local immune cell activity to control abnormal inflammation, helping restore balance within the joint environment and slow the progression of arthritis.
5. Clinical Applications and Outcomes
5.1 Observations and Study Results
Recent clinical studies and reviews show that PRP treatment can:
- Reduce Symptoms: Many early and moderate osteoarthritis patients experience less pain and improved joint movement after PRP injections.
- Support Repair: Compared to traditional medications, Platelet-Rich Plasma shows strong potential for promoting joint tissue repair while having fewer side effects.
However, some studies question the long-term effects of PRP. Large-scale, multicenter trials are still needed to verify its safety and effectiveness fully.
5.2 Suitable Cases and Limitations
- Ideal Candidates: PRP works best for patients with early to moderate arthritis or mild synovitis. Its benefits for advanced arthritis or severe joint damage are limited.
- Limitations: The treatment’s success can vary due to individual differences, preparation methods, injection frequency, and technique. A thorough evaluation by a qualified doctor is essential before starting treatment.
5.3 Clinical Practice Examples
In many hospitals, PRP has become part of comprehensive arthritis treatment programs. For example:
- A hospital combined Platelet-Rich Plasma injections with rehabilitation exercises for patients with moderate osteoarthritis, resulting in significant symptom relief and improved joint function.
- Some patients who received multiple PRP injections showed slower disease progression and enhanced quality of life in long-term follow-up.
These real-world cases support the potential of Platelet-Rich Plasma, although standard treatment protocols and more data are needed.
6. Frequently Asked Questions
6.1 Is PRP suitable for all arthritis patients?
PRP mainly benefits patients in the early to moderate stages of arthritis. Those with advanced or severely damaged joints often require additional treatments. It is important to consult a doctor to assess the condition before choosing PRP.
6.2 Is the PRP treatment process safe?
PRP uses the patient’s blood, which minimizes the risk of immune reactions. However, maintaining sterility during blood collection and injection is critical to prevent infections. Choosing experienced professionals and certified facilities ensures the treatment’s safety.
6.3 What should patients do after treatment?
After PRP treatment, patients should:
- Rest and avoid intense activities to protect the joint.
- Follow the doctor’s advice on rehabilitation and schedule regular check-ups.
- Monitor the injection site for any unusual reactions and seek medical help if needed.
7. Conclusion
PRP offers a promising alternative for managing arthritis by releasing growth factors and reducing inflammation to help repair joint tissues. This treatment shows great potential, especially for early and moderate cases. However, standardization, personalized protocols, and long-term studies remain essential to fully validate its benefits. With ongoing research and clinical practice, Platelet-Rich Plasma may soon play an even larger role in the comprehensive care of arthritis patients.
This article provides a clear, professional overview for both medical professionals and patients, while also meeting search engine optimization standards to improve visibility and indexing.